Volume 10, Issue 2 (4-2025)
CJHR 2025, 10(2): 121-132 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gorji M, Bakhshi F, omidi S, molaei L. Factors Related to Stress, Anxiety, and Depression in Northern Iran: Application of Health Locus of Control. CJHR 2025; 10 (2) :121-132
URL: http://cjhr.gums.ac.ir/article-1-398-en.html
URL: http://cjhr.gums.ac.ir/article-1-398-en.html
1- Research Center of Health and Environment, Guilan University of Medical Sciences, Rasht, Iran
2- Department of in Health Education and Health Promotion, School of Health, Guilan University of Medical Sciences, Rasht, Iran ,fa.bakhshi88@gmail.com
3- Department of Biostatistics and Epidemiology, School of Health, Guilan University of Medical Sciences, Rasht, Iran
2- Department of in Health Education and Health Promotion, School of Health, Guilan University of Medical Sciences, Rasht, Iran ,
3- Department of Biostatistics and Epidemiology, School of Health, Guilan University of Medical Sciences, Rasht, Iran
Full-Text [PDF 852 kb]
(208 Downloads)
| Abstract (HTML) (504 Views)
Full-Text: (142 Views)
Introduction
The prevalence of mental health disorders, including anxiety and depression, has become a significant global health concern, exacerbated by rising environmental stressors in various settings such as families, workplaces, and communities. In 2019, approximately one in eight people globally, or 970 million individuals, were living with a mental disorder, with anxiety and depression being the most common [1]. Depression affected 280 million people, including 23 million children and adolescents, in that same year [2]. The COVID-19 pandemic further intensified this mental health crisis, with a 26% increase in anxiety disorders and a 28% rise in major depression cases reported in 2020 [3]. By 2021, in the United States alone, 57.2 million individuals were diagnosed with anxiety and depression during medical visits [4].
Despite the growing burden of mental disorders, healthcare systems worldwide remain under-resourced and unable to adequately meet the demand for mental health care [2, 5]. For instance, only one-third of individuals with depression receive appropriate mental health interventions [6].
The variability in emotional responses to illness, including the levels of anxiety, depression, and stress, is influenced by individuals’ perceived control over their environment [7]. The concept of health locus of control (HLC) offers a theoretical framework to understand these variations. HLC predicts health-promoting behaviors based on whether individuals attribute their health outcomes to internal factors (personal actions) or external factors (luck or fate) [8, 9]. Those with an internal locus of control believe their actions shape their experiences and are more likely to engage in health-promoting behaviors, whereas individuals with an external locus of control may feel powerless and less motivated to influence their health [10].
The development of a strong internal locus of control is essential for fostering autonomy and resilience, which can enhance mental health outcomes. Interventions that promote internality, especially among populations at risk for mental disorders, may improve psychological well-being and reduce the incidence of anxiety, depression, and stress [9-11]. Understanding the relationship between locus of control and mental health is critical for developing effective strategies to address the global mental health crisis.
This study aimed to provide valuable insights for both participants and researchers by identifying association between internal and external locus of control on stress, anxiety, and depression. Understanding these factors will inform the development of more targeted and effective interventions to mitigate these psychological conditions. Grounded in the HLC theory, this research examines the associations between locus of control and mental health outcomes among individuals attending a comprehensive health center in a northern city of Iran. By elucidating the factors contributing to stress, anxiety, and depression, this study seeks to enhance future strategies for mental health management in similar populations.
Material and Methods
Study design and participants
This descriptive-analytical cross-sectional study utilized a questionnaire to investigate factors associated with stress, anxiety, and depression. The duration of data collection and questionnaire completion was approximately 70 days from October to December 2022. The study population comprised individuals aged 18 years and older who attended eight comprehensive health care centers in Northern Iran during the pandemic. The sample size was determined according to the distribution of dependent variables (e.g. depression, anxiety) in the target population. According to Falahzadeh et al. [12], the prevalence of depression, anxiety, and stress was 54.3%, 57.7%, and 51%, respectively. Considering a type I error rate of 5% and a precision level of 5%, the required sample size was calculated to be 384 participants. Participants were selected from households registered in the health centers, with sample sizes proportionally allocated based on the population each center served. Simple random sampling was applied using the Integrated Health Information Registration System (SIB). Participants were selected via random number generation based on their national codes recorded in the SIB system. The location for completing the questionnaire was the family health room of each center. The average time women took to complete the questionnaire was about ten minutes. Inclusion criteria included participants registered in the SIB system and the absence of any diagnosed stress, anxiety, or depression disorders. Individuals who failed to respond to the questionnaire were excluded from the study.
Data collection tools
Data were collected using a self-report questionnaire consisting of three parts:
Part A: Demographic characteristics
This section included 12 items assessing participants’ age, gender, education, marital status, number of children, occupation, household income, family composition, history of chronic illness, COVID-19 history, severity of illness, and hospitalization history due to COVID-19.
Part B: Depression, anxiety, and stress scale (DASS-21)
The DASS-21 is a validated tool that measures negative emotional states related to depression, anxiety, and stress, with seven items per subscale [13]. Responses were recorded on a 4-point Likert scale (1=“not true of me at all” to 4=“true of me most of the time”). Total scores for each subscale were classified as normal, mild, moderate, severe, or extremely severe. The DASS-21 has shown high reliability and suitable convergent validity [14]. Cronbach’s α for the DASS-21 in this study was 0.808, indicating strong reliability.
Part C: Multidimensional HLC (MHLC) scale
The MHLC scale assesses internal, external, and chance-based beliefs regarding health outcomes. The MHLC scale form C (form C MHLC scale) [15]. This form consists of 18 items and four subscales, including the internality part: Internal HLC (IHLC) (6 items), and the externality part: Chance HLC (CHLC) (6 items), powerful others contain doctors HLC (DHLC) (3 items), and other people HLC (OHLC) (3 items) and chance. The MHLC scale rated on a 6-point Likert scale (1=“strongly disagree” to 6=“strongly agree”), with higher scores reflecting stronger beliefs in the respective locus of control. The validity and reliability of this tool have been confirmed in prior study in Iran [16].
Statistical analysis
Descriptive statistics, including frequencies and percentages for categorical variables, and Means±SD for continuous variables, were used to characterize the study population. Normality of the data was assessed using the Shapiro-Wilk and Kolmogorov-Smirnov tests. Given that depression, anxiety, and stress scores, along with belief and chance subscales, were not normally distributed, non-parametric tests were employed. Spearman’s correlation analysis was used to assess the relationships between mental health outcomes and health control constructs. Logistic regression analyses were conducted to identify predictive factors associated with stress, anxiety, and depression. DASS scores above normal values i.e. >14, >9, and >7 were used to define the presence of stress, depression, and anxiety symptoms, respectively [17]. The goodness-of-fit of the logistic regression models was evaluated using the Hosmer-Lemeshow test. The proportion of variance explained by the independent variables in the regression models was quantified using R-squared (R²). Statistical analyses were performed using STATA software, version 17, with a significance level set at P<0.05.
Results
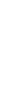
A total of 373 valid questionnaires were obtained and analyzed (participation rate=97%). The majority of participants were female (63.5%), and the mean age was 37.12±10.18 years, ranging from 18 to 77 years. Of the participants, 38.34% had attained a higher education level, 75.60% were married, 58.18% reported a history of COVID-19 infection, and 55.29% experienced moderate to severe cases of the illness. Additionally, 4.02% had been hospitalized due to COVID-19. The mean scores for internal health locus of control, belief in powerful others, and chance were 70.79±8.37, 27.97±4.14, 24.59±4.94, and 18.24±4.63, respectively (Table 1).
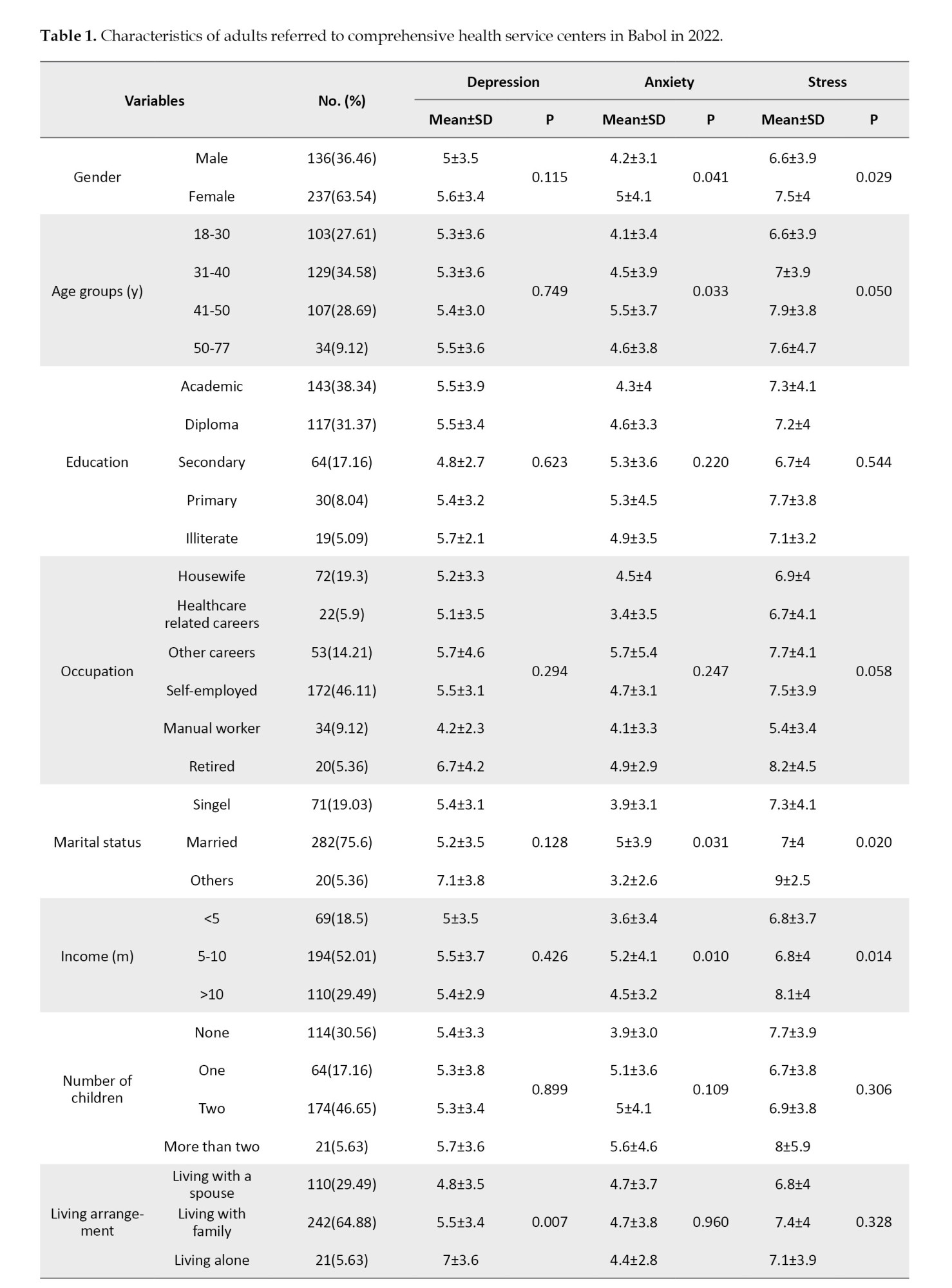

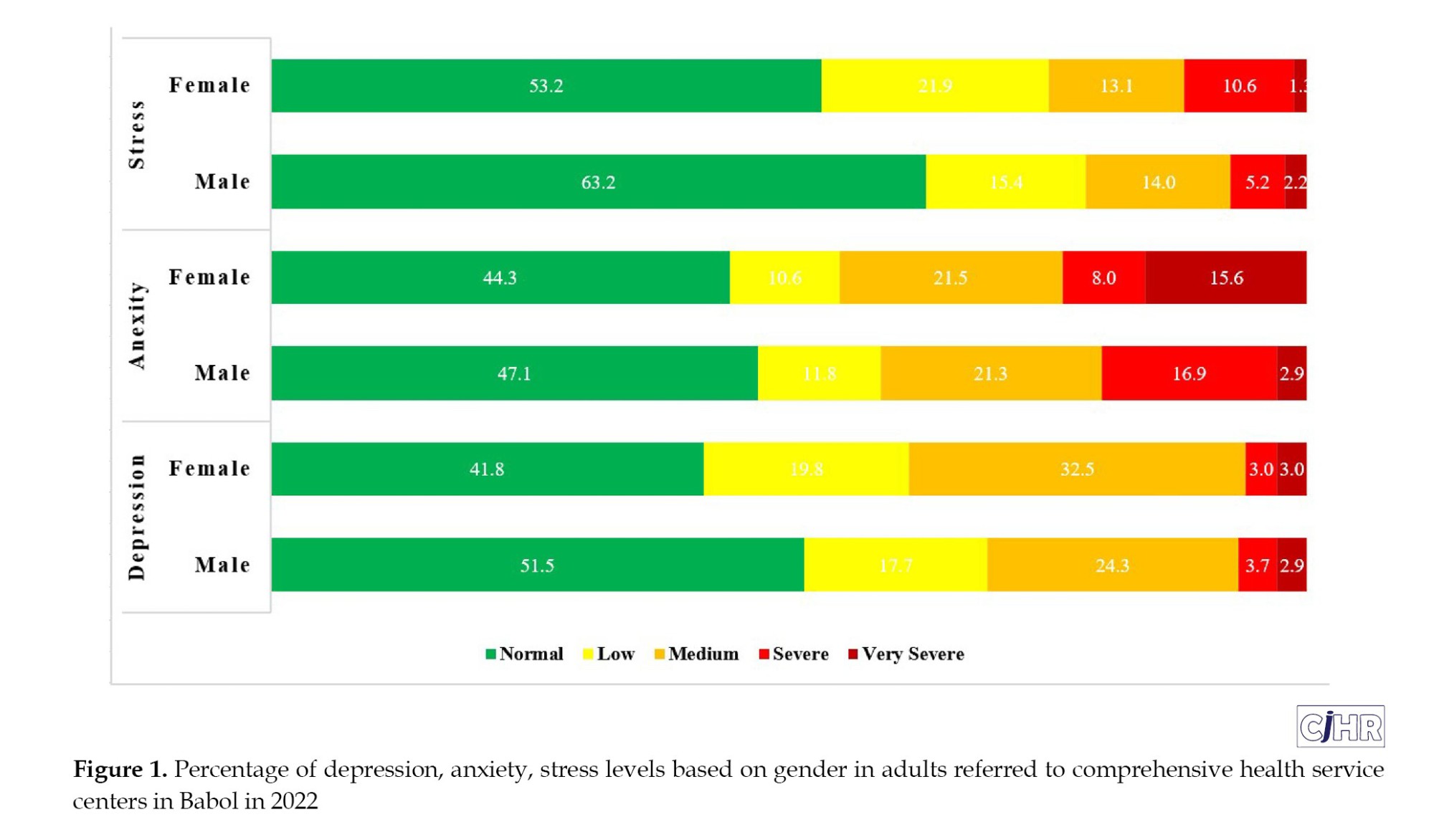
In terms of mental health symptoms, 54.7% of participants experienced higher than normal depression and anxiety scores, while 43.2% exhibited elevated than normal stress scores. Women reported higher levels of stress compared to men (P=0.02), and anxiety levels were significantly greater in females than in males (P=0.001) (Figure 1).
Among the participants, 25.7% reported experiencing concurrent symptoms of anxiety, depression, and stress. Additionally, 39.4% experienced both depression and anxiety, 34.9% experienced depression and stress, and 29.0% reported simultaneous stress and anxiety. Correlation analyses identified two statistically significant associations: Effective People inversely correlated with stress (r=-0.15, P=0.003), while chance positively correlated with anxiety (r=0.17, P=0.001). Non-significant weak associations included belief with all outcomes (depression: r=-0.04, P=0.44; anxiety: r=-0.00, P=0.99; stress: r=0.03, P=0.52), Effective People with depression (r=-0.07, P=0.16) and anxiety (r=0.01, P=0.93), and chance with depression (r=0.06, P=0.22) and stress (r=0.08, P=0.10).
Mann-Whitney U test and Kruskal-Walli’s test revealed significant associations between depression and living arrangements as well as COVID-19-related hospitalization. Anxiety was significantly associated with age, marital status, and income. Stress was linked to age, gender, income, marital status, the presence of chronic disease, COVID-19 severity, and COVID-19-related hospitalization (Table 1).
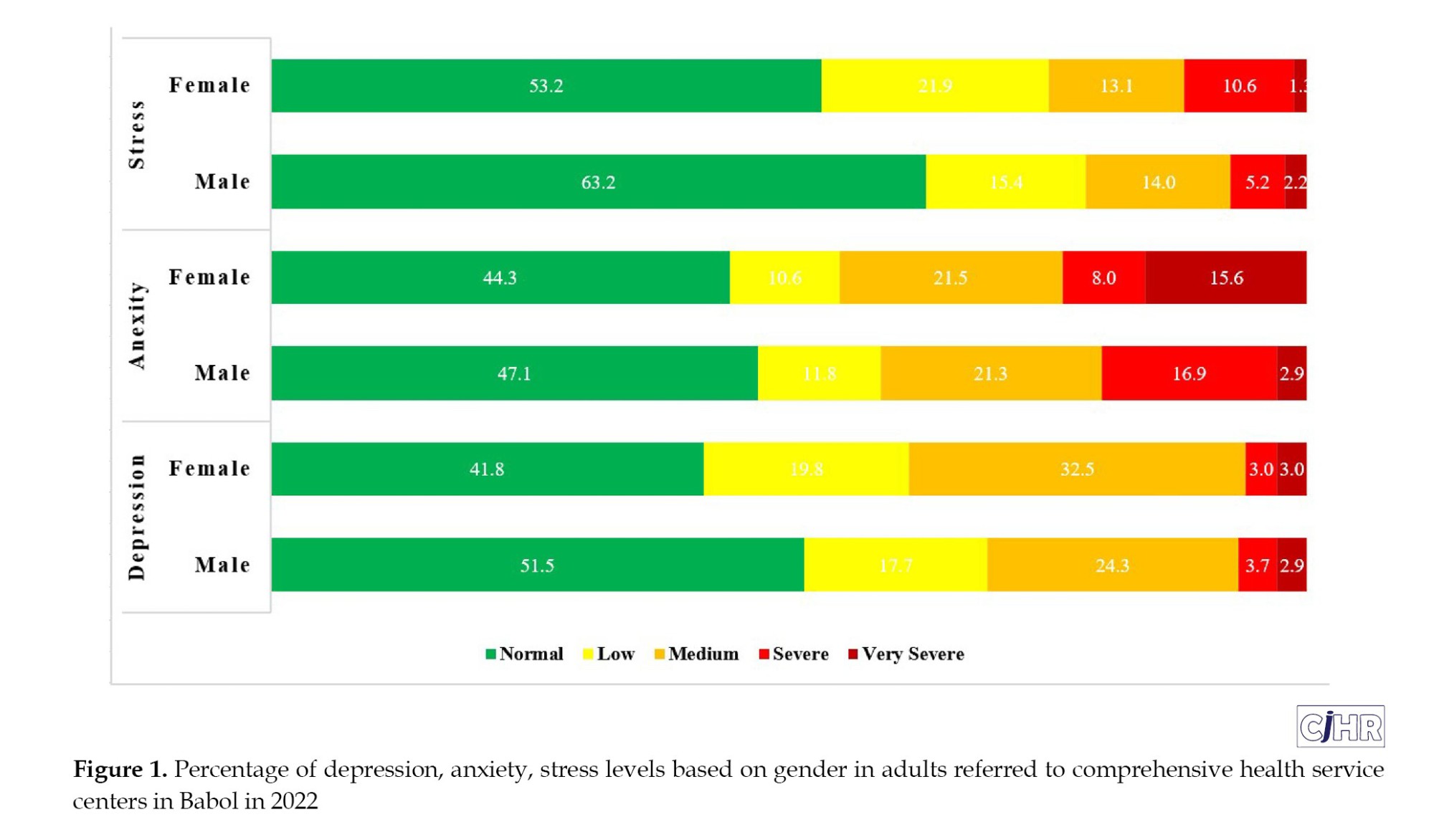
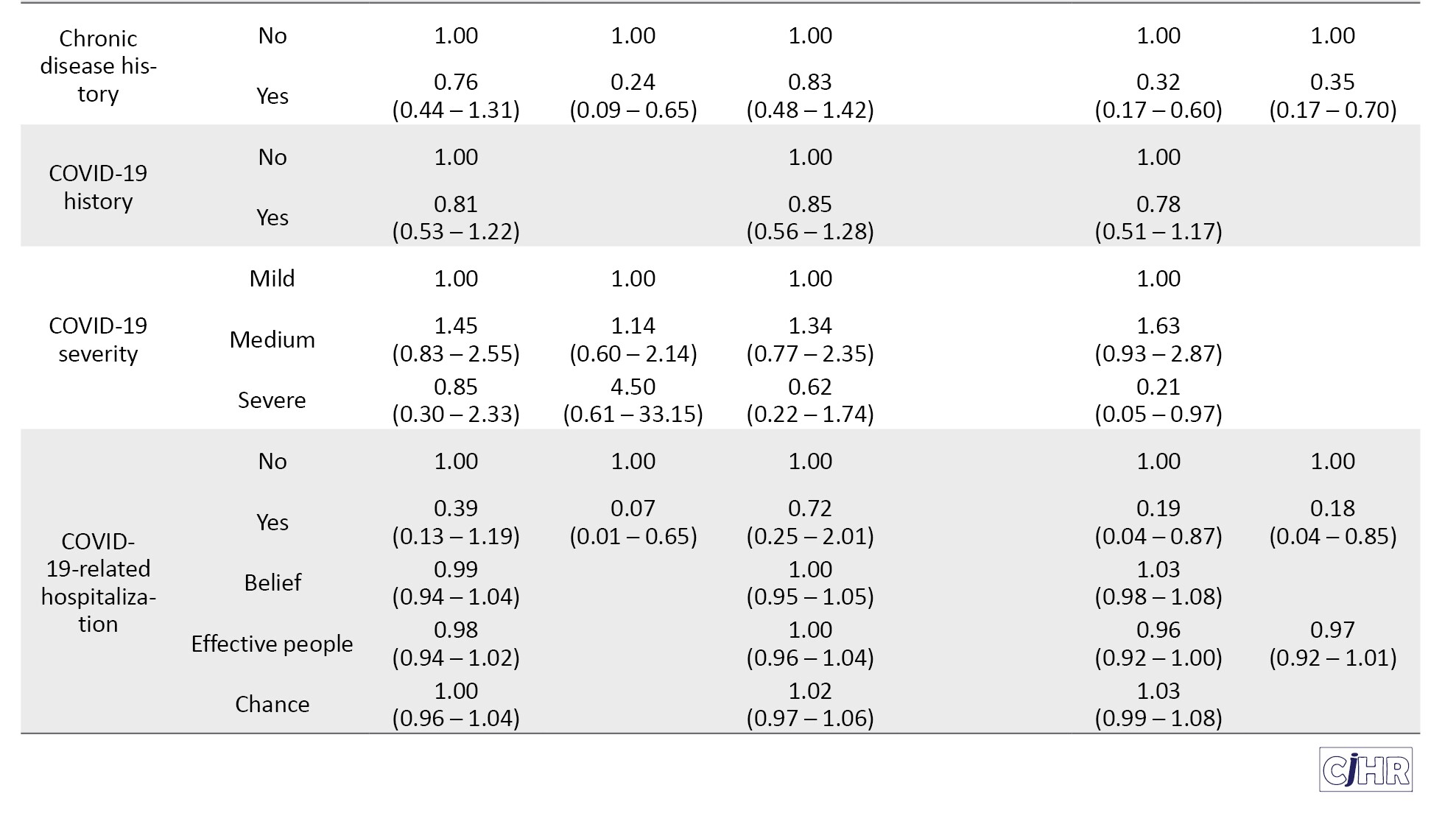
Depression
In the crude logistic regression analysis, living alone (OR=4.13) and living with family (OR=1.77) were associated with increased odds of depression compared to living with a spouse. In the adjusted model, the odds of depression increased with the number of children (1 child: OR=3.21; 2 children: OR=3.07; >2 children: OR=78.82), compared to having no children. Conversely, a history of chronic disease (OR=0.24) and COVID-19-related hospitalization (OR=0.07) were associated with reduced odds of depression (Table 2).
Anxiety
Crude logistic regression analysis indicated that anxiety was significantly associated with being aged 41-50 (OR=1.86) compared to ages 18-30, having a high school diploma (OR=1.80) or secondary education (OR=2.23) compared to academic education, and being retired (OR=3.55) or self-employed (OR=1.76) compared to housewives. Having one child (OR=1.74) or two children (OR=1.69) also increased the odds of anxiety compared to having no children. Adjusted analysis further revealed that anxiety was significantly associated with being female (OR=1.80), having secondary education (OR=2.47) compared to academic education, being retired (OR=4.12) or self-employed (OR=2.47), having one child (OR=2.53) or two children (OR=1.85),and Individuals with an income ranging from 5 to 10 million per month exhibited lower odds of experiencing anxiety (0.41) compared to those earning less than 5 million per month. Interestingly, income below 5 million IRR was associated with lower odds of anxiety (Table 2).
Stress
Crude analysis showed that stress was significantly associated with being female (OR=1.52), aged 41-50 (OR=2.23), and having a marital status categorized as “other” (divorced or widowed) (OR=3.87). In contrast, factors associated with lower odds of stress included having an income above 10 million IRR (OR=0.57), the presence of chronic diseases (OR=0.32), moderate COVID-19 severity (OR=1.63), severe COVID-19 (OR=0.21), and COVID-19-related hospitalization (OR=0.19). The adjusted analysis confirmed that individuals aged 41-50 (OR=2.40), and those divorced or widowed (OR=43.46) had significantly higher odds of experiencing stress. chronic disease history (OR=0.35) and COVID-19-related hospitalization (OR=0.18) were associated with lower odds of stress (Table 2).
Discussion
This study aimed to investigate the factors associated with stress, anxiety, and depression within the framework of the HLC theory. The findings revealed that 43.2% of participants reported experiencing stress score above the normal value, 54.7% exhibited mild to severe anxiety and depression. These prevalence rates align with similar studies conducted during the COVID-19 pandemic. For instance, Varma et al. reported that 70% of the Australian general population experienced stress, 59% anxiety, and 39% depression during April-May 2020 [18]. Likewise, Kavvadas et al. found that university students in northern Greece experienced increasing levels of stress, anxiety, and depression from November 2020 to November 2021 [19]. These findings underscore the pervasive psychological impact of the COVID-19 pandemic across different populations.
The prevalence of psychological distress observed in the current study may be attributed to the timing of data collection during a period of uncertainty related to the pandemic. Previous studies have demonstrated a strong link between infectious disease outbreaks time and elevated anxiety, stress, and post-traumatic symptoms [20-22]. A study in the Iranian population showed that acceptance of the COVID-19 vaccine decreased after the ninth wave in February 2021 [23]. Given that the current study coincides with after that period, psychological issues were slightly adjusted. Stress, anxiety, and depression are often a response to perceived uncontrollable external threats, which may explain why the pandemic exacerbated these mental health issues across different demographics.
Health locus of control and psychological outcomes
Our analysis of the dimensions of the HLC revealed that participants had the highest scores for internal control, followed by external control dimensions such as powerful others and chance. The dominance of internal control belief is consistent with previous studies [11]. Ganjoo et al. found that internal HLC (IHLC) was the most prominent component among students [24]. But the findings of our study failed to show any association between HLC and dimensions of mental health. In contrast of our findings, Alat et al. reported that individuals with a strong internal control orientation evaluated their health more positively and had better physical and mental health [25], Holden et al. found an inverse relationship between perceived stress and internal locus of control among students, suggesting that individuals who believe they can control their life events tend to experience lower stress [26]. Additionally, Khumalo et al. observed that students with a stronger internal locus of control were less likely to experience depressive symptoms [27]. These findings highlight some degree of the protective role of internal control in reducing stress, anxiety, and depression in other studies. The lack of significant associations between HLC and mental health components in the present study could be due to demographic, cultural, or measurement differences. While it has been suggested that HLC is a suitable theory for mental health interventions, it seems that replication of studies similar to our study in other societies and cultures could shed light on the contradictions that have arisen.
Demographic correlates of stress, anxiety, and depression
Our findings show that women, divorced or single individuals, and those with higher household incomes reported significantly higher levels of stress, whereas individuals with chronic illness or a history of hospitalization due to COVID-19 experienced lower stress. These results are consistent with Ghanbari Afra’s study, which also identified significant relationships between demographic variables and stress levels [28]. Additionally, higher anxiety levels were reported among individuals aged 40-51 years and married participants, mirroring results from studies conducted in Pakistan [29] and Iran [30]. However, discrepancies exist when compared to studies from Poland [31] and Korea [32], indicating potential cultural or contextual differences in the expression and management of anxiety.
Living arrangements and hospitalization due to COVID-19 or its complications were significantly associated with depression. Participants living alone reported higher levels of depression, whereas those living with a spouse experienced lower depression levels. This finding aligns with the literature suggesting that social support, particularly from a spouse, can buffer against depressive symptoms during stressful events [33-36]. In contrast, individuals with a history of severe illness or hospitalization face increased risk for depression, likely due to the long-term psychological impact of severe health challenges [37].
Health locus of control and stress
An important finding of this study was the significant inverse relationship between stress and the external health locus of control. Participants who attributed their health outcomes to external factors, particularly powerful others, reported lower stress levels. This is in contrast to studies such as those by Miličić et al., which found that patients with acute heart conditions exhibited higher external control beliefs and poorer psychological outcomes [38]. Similarly, de Dios-Duarte et al. reported that Crohn’s disease patients with higher external control experienced elevated stress [39]. These divergent findings suggest that the role of external control in stress management may vary based on specific health conditions and personal beliefs.
Depression did not exhibit significant associations with any of the HLC dimensions in our study. However, a meta-analysis indicated that external health control is generally correlated with anxiety and depression, while internal health control is inversely related to depression levels [40]. This inconsistency could be attributed to cultural differences or the unique stressors related to the pandemic, which may alter the typical relationships between control beliefs and mental health outcomes.
Implications for mental health interventions
The findings of this study suggest that fostering an internal HLC could be a valuable strategy in mitigating stress, anxiety, and depression. Individuals who believe they can influence their health through their actions are more likely to engage in health-promoting behaviors and demonstrate resilience in the face of stressors [41]. Given the strong relationship between control beliefs and psychological outcomes, mental health interventions should focus on strengthening individuals’ internal locus of control through cognitive-behavioral techniques and psychoeducation.
Furthermore, demographic factors such as gender, marital status, and socioeconomic status play a critical role in mental health outcomes. Targeted interventions addressing the unique stressors faced by these groups may be particularly effective in reducing psychological distress.
Conclusion
The HLC is a key psychological factor influencing how individuals respond to stress, anxiety, and depression. Although the results of this study failed to show a strong predictor of HLC for stress, anxiety, and depression, promoting an internal locus of control through counseling and educational programs could enhance mental health and well-being overally, particularly during times of crisis like the COVID-19 pandemic. Understanding the demographic and psychosocial correlates of mental health outcomes can inform more tailored and effective interventions, ultimately improving individuals’ ability to manage stress and maintain psychological resilience.
The study applies the HLC framework to explore psychological distress, offering unique insights, including valuable information on how demographic factors influence mental health. Causality cannot be determined due to the study’s cross-sectional nature. Self-reported data may also be influenced by bias, affecting accuracy. Therefore, similar studies with other method, models and theories are suggestedEthical Considerations
Compliance with ethical guidelines
This study was approved by the Scientific and Ethical Committees of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.334).
Funding
The paper was extracted from the master's thesis of Melika Gorji, approved by the Department of Health Education and Health Promotion, School of Health School, University of Guilan University of Medical Sciences, Rasht, Iran.
Authors' contributions
Conceptualization and study design: Fataneh Bakhshi and Saeed Omidi; Data analysis, interpretation, and writing the original draft: All authors; Review and editing: Fataneh Bakhshi and Leila Molaeipour; Statistical analysis: Melika Gorji and Leila Molaeipour.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors extend their sincere gratitude to the Vice-Chancellor for Research at Guilan University of Medical Sciences, Rasht, Iran, for approving and funding this research. The authors also thank their colleagues at the Babol Comprehensive Health Centers for their invaluable support, as well as all participants who generously volunteered their time and effort during this study.
References
The prevalence of mental health disorders, including anxiety and depression, has become a significant global health concern, exacerbated by rising environmental stressors in various settings such as families, workplaces, and communities. In 2019, approximately one in eight people globally, or 970 million individuals, were living with a mental disorder, with anxiety and depression being the most common [1]. Depression affected 280 million people, including 23 million children and adolescents, in that same year [2]. The COVID-19 pandemic further intensified this mental health crisis, with a 26% increase in anxiety disorders and a 28% rise in major depression cases reported in 2020 [3]. By 2021, in the United States alone, 57.2 million individuals were diagnosed with anxiety and depression during medical visits [4].
Despite the growing burden of mental disorders, healthcare systems worldwide remain under-resourced and unable to adequately meet the demand for mental health care [2, 5]. For instance, only one-third of individuals with depression receive appropriate mental health interventions [6].
The variability in emotional responses to illness, including the levels of anxiety, depression, and stress, is influenced by individuals’ perceived control over their environment [7]. The concept of health locus of control (HLC) offers a theoretical framework to understand these variations. HLC predicts health-promoting behaviors based on whether individuals attribute their health outcomes to internal factors (personal actions) or external factors (luck or fate) [8, 9]. Those with an internal locus of control believe their actions shape their experiences and are more likely to engage in health-promoting behaviors, whereas individuals with an external locus of control may feel powerless and less motivated to influence their health [10].
The development of a strong internal locus of control is essential for fostering autonomy and resilience, which can enhance mental health outcomes. Interventions that promote internality, especially among populations at risk for mental disorders, may improve psychological well-being and reduce the incidence of anxiety, depression, and stress [9-11]. Understanding the relationship between locus of control and mental health is critical for developing effective strategies to address the global mental health crisis.
This study aimed to provide valuable insights for both participants and researchers by identifying association between internal and external locus of control on stress, anxiety, and depression. Understanding these factors will inform the development of more targeted and effective interventions to mitigate these psychological conditions. Grounded in the HLC theory, this research examines the associations between locus of control and mental health outcomes among individuals attending a comprehensive health center in a northern city of Iran. By elucidating the factors contributing to stress, anxiety, and depression, this study seeks to enhance future strategies for mental health management in similar populations.
Material and Methods
Study design and participants
This descriptive-analytical cross-sectional study utilized a questionnaire to investigate factors associated with stress, anxiety, and depression. The duration of data collection and questionnaire completion was approximately 70 days from October to December 2022. The study population comprised individuals aged 18 years and older who attended eight comprehensive health care centers in Northern Iran during the pandemic. The sample size was determined according to the distribution of dependent variables (e.g. depression, anxiety) in the target population. According to Falahzadeh et al. [12], the prevalence of depression, anxiety, and stress was 54.3%, 57.7%, and 51%, respectively. Considering a type I error rate of 5% and a precision level of 5%, the required sample size was calculated to be 384 participants. Participants were selected from households registered in the health centers, with sample sizes proportionally allocated based on the population each center served. Simple random sampling was applied using the Integrated Health Information Registration System (SIB). Participants were selected via random number generation based on their national codes recorded in the SIB system. The location for completing the questionnaire was the family health room of each center. The average time women took to complete the questionnaire was about ten minutes. Inclusion criteria included participants registered in the SIB system and the absence of any diagnosed stress, anxiety, or depression disorders. Individuals who failed to respond to the questionnaire were excluded from the study.
Data collection tools
Data were collected using a self-report questionnaire consisting of three parts:
Part A: Demographic characteristics
This section included 12 items assessing participants’ age, gender, education, marital status, number of children, occupation, household income, family composition, history of chronic illness, COVID-19 history, severity of illness, and hospitalization history due to COVID-19.
Part B: Depression, anxiety, and stress scale (DASS-21)
The DASS-21 is a validated tool that measures negative emotional states related to depression, anxiety, and stress, with seven items per subscale [13]. Responses were recorded on a 4-point Likert scale (1=“not true of me at all” to 4=“true of me most of the time”). Total scores for each subscale were classified as normal, mild, moderate, severe, or extremely severe. The DASS-21 has shown high reliability and suitable convergent validity [14]. Cronbach’s α for the DASS-21 in this study was 0.808, indicating strong reliability.
Part C: Multidimensional HLC (MHLC) scale
The MHLC scale assesses internal, external, and chance-based beliefs regarding health outcomes. The MHLC scale form C (form C MHLC scale) [15]. This form consists of 18 items and four subscales, including the internality part: Internal HLC (IHLC) (6 items), and the externality part: Chance HLC (CHLC) (6 items), powerful others contain doctors HLC (DHLC) (3 items), and other people HLC (OHLC) (3 items) and chance. The MHLC scale rated on a 6-point Likert scale (1=“strongly disagree” to 6=“strongly agree”), with higher scores reflecting stronger beliefs in the respective locus of control. The validity and reliability of this tool have been confirmed in prior study in Iran [16].
Statistical analysis
Descriptive statistics, including frequencies and percentages for categorical variables, and Means±SD for continuous variables, were used to characterize the study population. Normality of the data was assessed using the Shapiro-Wilk and Kolmogorov-Smirnov tests. Given that depression, anxiety, and stress scores, along with belief and chance subscales, were not normally distributed, non-parametric tests were employed. Spearman’s correlation analysis was used to assess the relationships between mental health outcomes and health control constructs. Logistic regression analyses were conducted to identify predictive factors associated with stress, anxiety, and depression. DASS scores above normal values i.e. >14, >9, and >7 were used to define the presence of stress, depression, and anxiety symptoms, respectively [17]. The goodness-of-fit of the logistic regression models was evaluated using the Hosmer-Lemeshow test. The proportion of variance explained by the independent variables in the regression models was quantified using R-squared (R²). Statistical analyses were performed using STATA software, version 17, with a significance level set at P<0.05.
Results
A total of 373 valid questionnaires were obtained and analyzed (participation rate=97%). The majority of participants were female (63.5%), and the mean age was 37.12±10.18 years, ranging from 18 to 77 years. Of the participants, 38.34% had attained a higher education level, 75.60% were married, 58.18% reported a history of COVID-19 infection, and 55.29% experienced moderate to severe cases of the illness. Additionally, 4.02% had been hospitalized due to COVID-19. The mean scores for internal health locus of control, belief in powerful others, and chance were 70.79±8.37, 27.97±4.14, 24.59±4.94, and 18.24±4.63, respectively (Table 1).
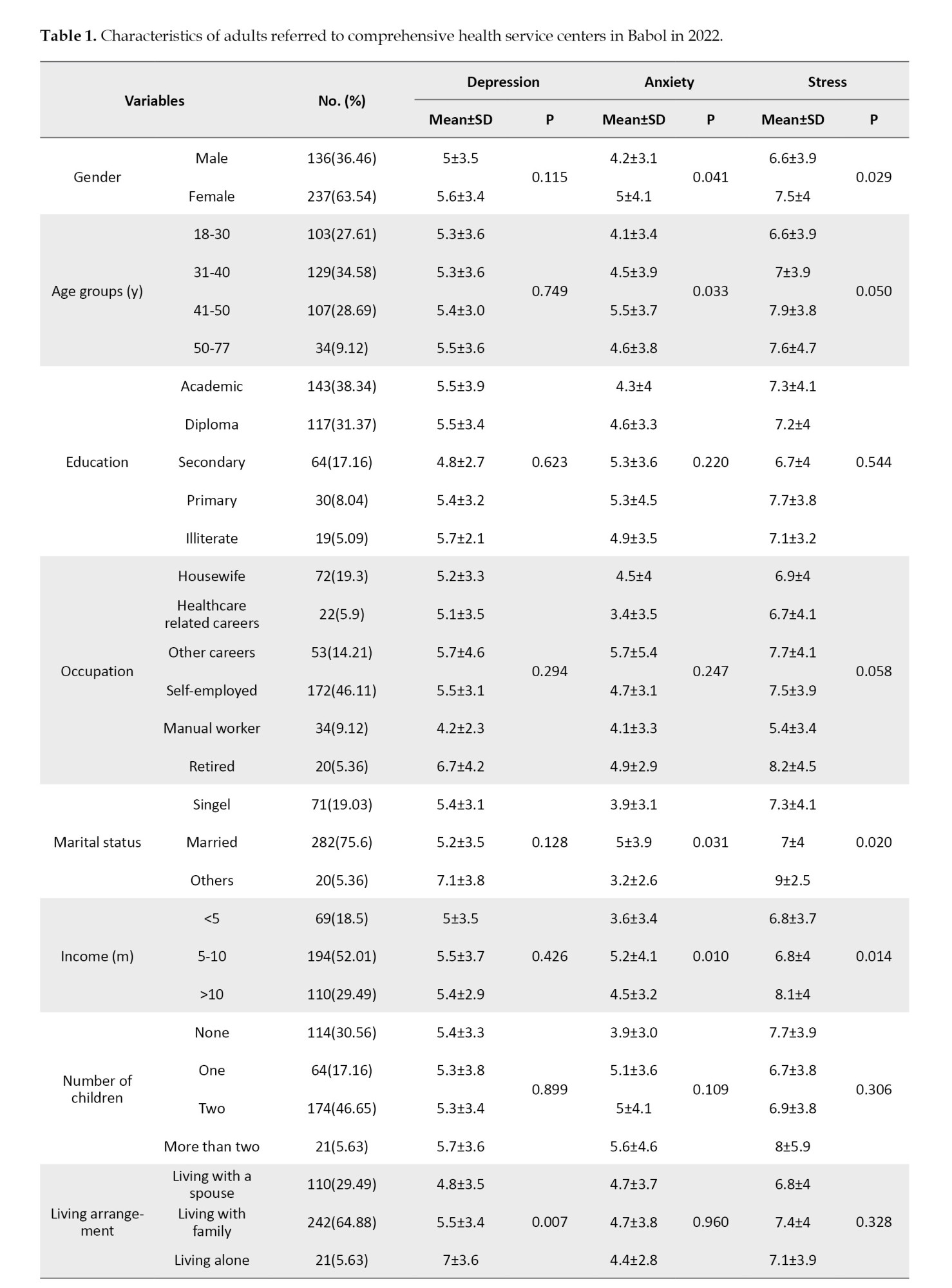

In terms of mental health symptoms, 54.7% of participants experienced higher than normal depression and anxiety scores, while 43.2% exhibited elevated than normal stress scores. Women reported higher levels of stress compared to men (P=0.02), and anxiety levels were significantly greater in females than in males (P=0.001) (Figure 1).
Among the participants, 25.7% reported experiencing concurrent symptoms of anxiety, depression, and stress. Additionally, 39.4% experienced both depression and anxiety, 34.9% experienced depression and stress, and 29.0% reported simultaneous stress and anxiety. Correlation analyses identified two statistically significant associations: Effective People inversely correlated with stress (r=-0.15, P=0.003), while chance positively correlated with anxiety (r=0.17, P=0.001). Non-significant weak associations included belief with all outcomes (depression: r=-0.04, P=0.44; anxiety: r=-0.00, P=0.99; stress: r=0.03, P=0.52), Effective People with depression (r=-0.07, P=0.16) and anxiety (r=0.01, P=0.93), and chance with depression (r=0.06, P=0.22) and stress (r=0.08, P=0.10).
Mann-Whitney U test and Kruskal-Walli’s test revealed significant associations between depression and living arrangements as well as COVID-19-related hospitalization. Anxiety was significantly associated with age, marital status, and income. Stress was linked to age, gender, income, marital status, the presence of chronic disease, COVID-19 severity, and COVID-19-related hospitalization (Table 1).
Depression
In the crude logistic regression analysis, living alone (OR=4.13) and living with family (OR=1.77) were associated with increased odds of depression compared to living with a spouse. In the adjusted model, the odds of depression increased with the number of children (1 child: OR=3.21; 2 children: OR=3.07; >2 children: OR=78.82), compared to having no children. Conversely, a history of chronic disease (OR=0.24) and COVID-19-related hospitalization (OR=0.07) were associated with reduced odds of depression (Table 2).
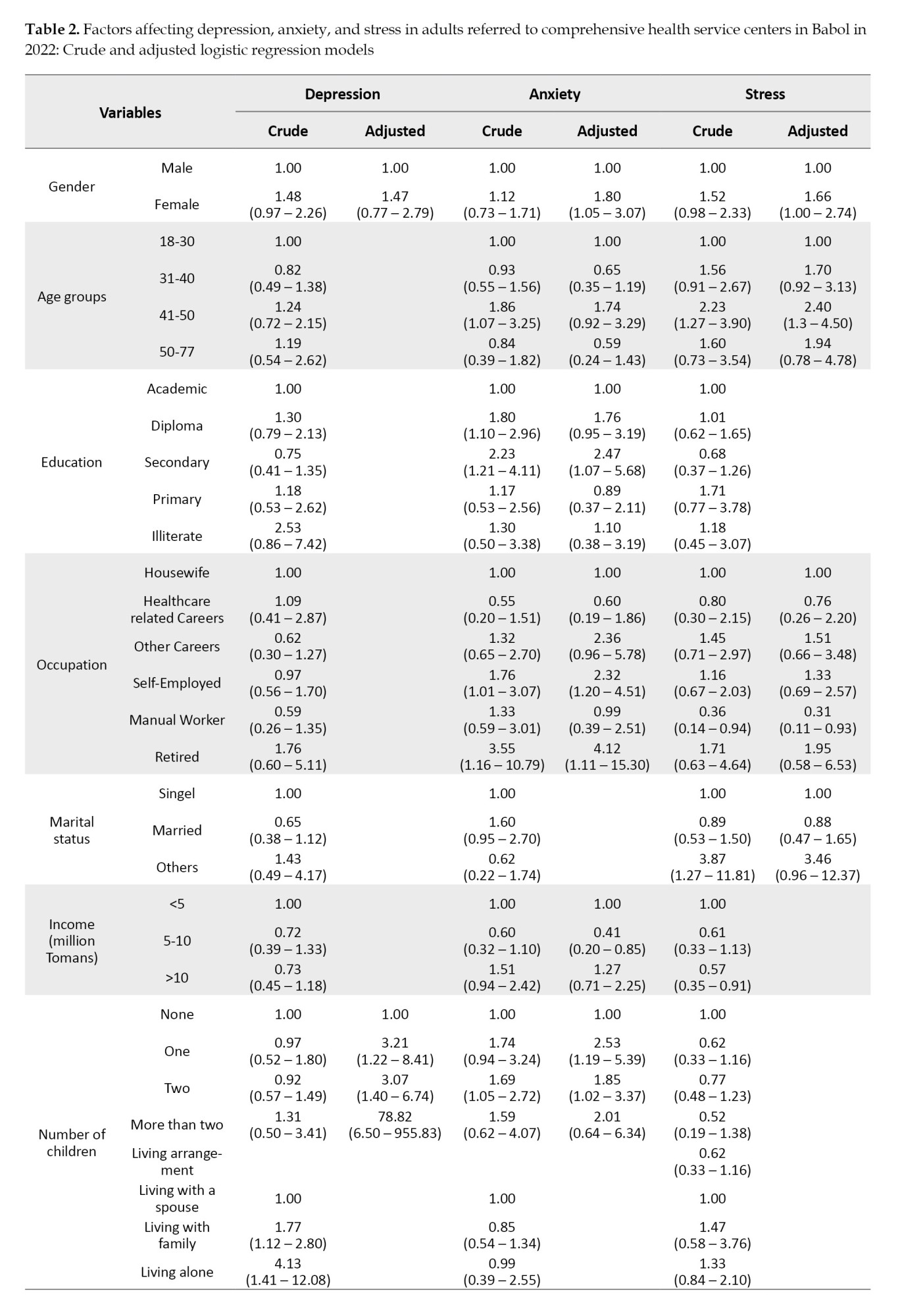
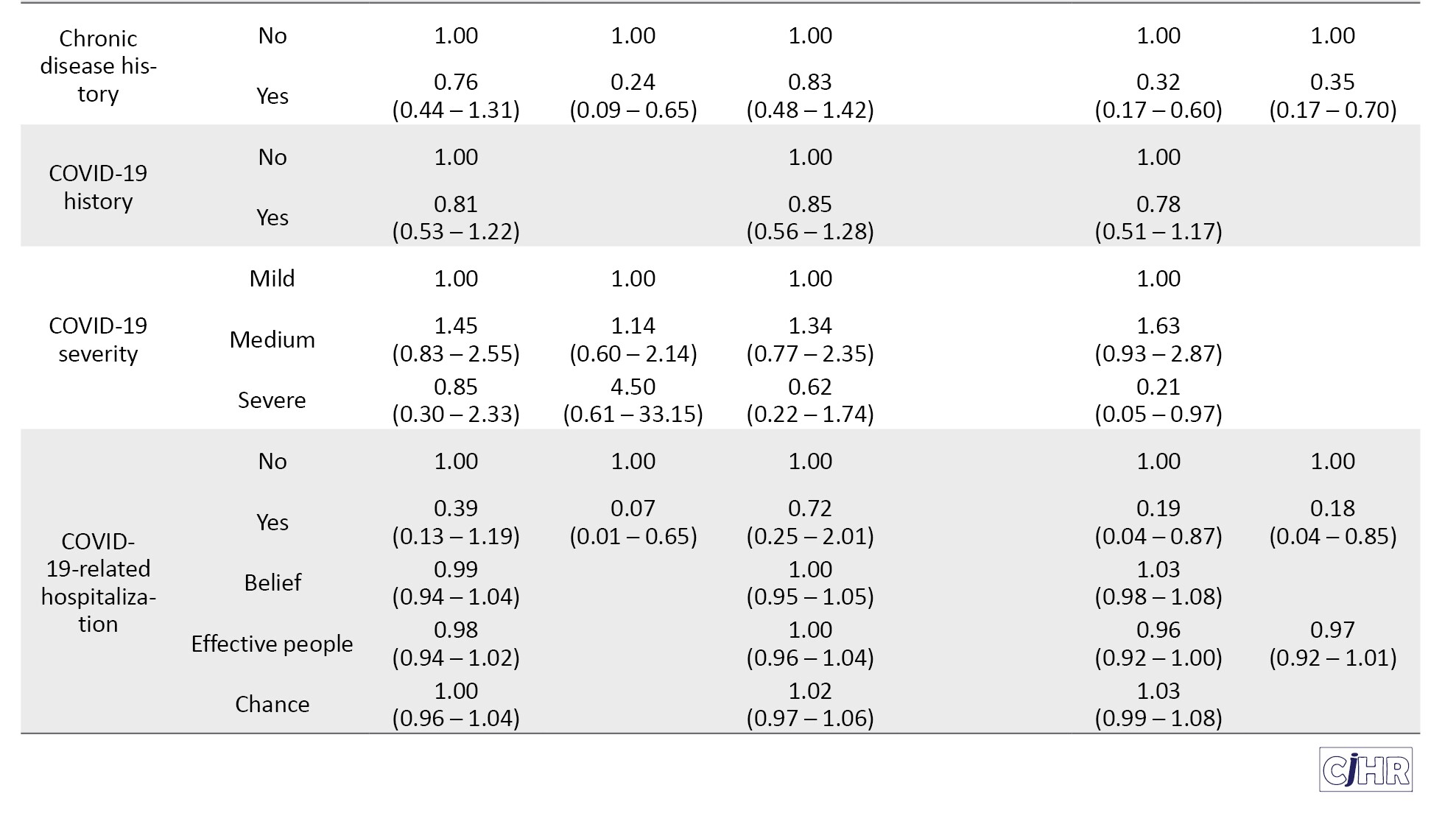
Anxiety
Crude logistic regression analysis indicated that anxiety was significantly associated with being aged 41-50 (OR=1.86) compared to ages 18-30, having a high school diploma (OR=1.80) or secondary education (OR=2.23) compared to academic education, and being retired (OR=3.55) or self-employed (OR=1.76) compared to housewives. Having one child (OR=1.74) or two children (OR=1.69) also increased the odds of anxiety compared to having no children. Adjusted analysis further revealed that anxiety was significantly associated with being female (OR=1.80), having secondary education (OR=2.47) compared to academic education, being retired (OR=4.12) or self-employed (OR=2.47), having one child (OR=2.53) or two children (OR=1.85),and Individuals with an income ranging from 5 to 10 million per month exhibited lower odds of experiencing anxiety (0.41) compared to those earning less than 5 million per month. Interestingly, income below 5 million IRR was associated with lower odds of anxiety (Table 2).
Stress
Crude analysis showed that stress was significantly associated with being female (OR=1.52), aged 41-50 (OR=2.23), and having a marital status categorized as “other” (divorced or widowed) (OR=3.87). In contrast, factors associated with lower odds of stress included having an income above 10 million IRR (OR=0.57), the presence of chronic diseases (OR=0.32), moderate COVID-19 severity (OR=1.63), severe COVID-19 (OR=0.21), and COVID-19-related hospitalization (OR=0.19). The adjusted analysis confirmed that individuals aged 41-50 (OR=2.40), and those divorced or widowed (OR=43.46) had significantly higher odds of experiencing stress. chronic disease history (OR=0.35) and COVID-19-related hospitalization (OR=0.18) were associated with lower odds of stress (Table 2).
Discussion
This study aimed to investigate the factors associated with stress, anxiety, and depression within the framework of the HLC theory. The findings revealed that 43.2% of participants reported experiencing stress score above the normal value, 54.7% exhibited mild to severe anxiety and depression. These prevalence rates align with similar studies conducted during the COVID-19 pandemic. For instance, Varma et al. reported that 70% of the Australian general population experienced stress, 59% anxiety, and 39% depression during April-May 2020 [18]. Likewise, Kavvadas et al. found that university students in northern Greece experienced increasing levels of stress, anxiety, and depression from November 2020 to November 2021 [19]. These findings underscore the pervasive psychological impact of the COVID-19 pandemic across different populations.
The prevalence of psychological distress observed in the current study may be attributed to the timing of data collection during a period of uncertainty related to the pandemic. Previous studies have demonstrated a strong link between infectious disease outbreaks time and elevated anxiety, stress, and post-traumatic symptoms [20-22]. A study in the Iranian population showed that acceptance of the COVID-19 vaccine decreased after the ninth wave in February 2021 [23]. Given that the current study coincides with after that period, psychological issues were slightly adjusted. Stress, anxiety, and depression are often a response to perceived uncontrollable external threats, which may explain why the pandemic exacerbated these mental health issues across different demographics.
Health locus of control and psychological outcomes
Our analysis of the dimensions of the HLC revealed that participants had the highest scores for internal control, followed by external control dimensions such as powerful others and chance. The dominance of internal control belief is consistent with previous studies [11]. Ganjoo et al. found that internal HLC (IHLC) was the most prominent component among students [24]. But the findings of our study failed to show any association between HLC and dimensions of mental health. In contrast of our findings, Alat et al. reported that individuals with a strong internal control orientation evaluated their health more positively and had better physical and mental health [25], Holden et al. found an inverse relationship between perceived stress and internal locus of control among students, suggesting that individuals who believe they can control their life events tend to experience lower stress [26]. Additionally, Khumalo et al. observed that students with a stronger internal locus of control were less likely to experience depressive symptoms [27]. These findings highlight some degree of the protective role of internal control in reducing stress, anxiety, and depression in other studies. The lack of significant associations between HLC and mental health components in the present study could be due to demographic, cultural, or measurement differences. While it has been suggested that HLC is a suitable theory for mental health interventions, it seems that replication of studies similar to our study in other societies and cultures could shed light on the contradictions that have arisen.
Demographic correlates of stress, anxiety, and depression
Our findings show that women, divorced or single individuals, and those with higher household incomes reported significantly higher levels of stress, whereas individuals with chronic illness or a history of hospitalization due to COVID-19 experienced lower stress. These results are consistent with Ghanbari Afra’s study, which also identified significant relationships between demographic variables and stress levels [28]. Additionally, higher anxiety levels were reported among individuals aged 40-51 years and married participants, mirroring results from studies conducted in Pakistan [29] and Iran [30]. However, discrepancies exist when compared to studies from Poland [31] and Korea [32], indicating potential cultural or contextual differences in the expression and management of anxiety.
Living arrangements and hospitalization due to COVID-19 or its complications were significantly associated with depression. Participants living alone reported higher levels of depression, whereas those living with a spouse experienced lower depression levels. This finding aligns with the literature suggesting that social support, particularly from a spouse, can buffer against depressive symptoms during stressful events [33-36]. In contrast, individuals with a history of severe illness or hospitalization face increased risk for depression, likely due to the long-term psychological impact of severe health challenges [37].
Health locus of control and stress
An important finding of this study was the significant inverse relationship between stress and the external health locus of control. Participants who attributed their health outcomes to external factors, particularly powerful others, reported lower stress levels. This is in contrast to studies such as those by Miličić et al., which found that patients with acute heart conditions exhibited higher external control beliefs and poorer psychological outcomes [38]. Similarly, de Dios-Duarte et al. reported that Crohn’s disease patients with higher external control experienced elevated stress [39]. These divergent findings suggest that the role of external control in stress management may vary based on specific health conditions and personal beliefs.
Depression did not exhibit significant associations with any of the HLC dimensions in our study. However, a meta-analysis indicated that external health control is generally correlated with anxiety and depression, while internal health control is inversely related to depression levels [40]. This inconsistency could be attributed to cultural differences or the unique stressors related to the pandemic, which may alter the typical relationships between control beliefs and mental health outcomes.
Implications for mental health interventions
The findings of this study suggest that fostering an internal HLC could be a valuable strategy in mitigating stress, anxiety, and depression. Individuals who believe they can influence their health through their actions are more likely to engage in health-promoting behaviors and demonstrate resilience in the face of stressors [41]. Given the strong relationship between control beliefs and psychological outcomes, mental health interventions should focus on strengthening individuals’ internal locus of control through cognitive-behavioral techniques and psychoeducation.
Furthermore, demographic factors such as gender, marital status, and socioeconomic status play a critical role in mental health outcomes. Targeted interventions addressing the unique stressors faced by these groups may be particularly effective in reducing psychological distress.
Conclusion
The HLC is a key psychological factor influencing how individuals respond to stress, anxiety, and depression. Although the results of this study failed to show a strong predictor of HLC for stress, anxiety, and depression, promoting an internal locus of control through counseling and educational programs could enhance mental health and well-being overally, particularly during times of crisis like the COVID-19 pandemic. Understanding the demographic and psychosocial correlates of mental health outcomes can inform more tailored and effective interventions, ultimately improving individuals’ ability to manage stress and maintain psychological resilience.
The study applies the HLC framework to explore psychological distress, offering unique insights, including valuable information on how demographic factors influence mental health. Causality cannot be determined due to the study’s cross-sectional nature. Self-reported data may also be influenced by bias, affecting accuracy. Therefore, similar studies with other method, models and theories are suggestedEthical Considerations
Compliance with ethical guidelines
This study was approved by the Scientific and Ethical Committees of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.334).
Funding
The paper was extracted from the master's thesis of Melika Gorji, approved by the Department of Health Education and Health Promotion, School of Health School, University of Guilan University of Medical Sciences, Rasht, Iran.
Authors' contributions
Conceptualization and study design: Fataneh Bakhshi and Saeed Omidi; Data analysis, interpretation, and writing the original draft: All authors; Review and editing: Fataneh Bakhshi and Leila Molaeipour; Statistical analysis: Melika Gorji and Leila Molaeipour.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors extend their sincere gratitude to the Vice-Chancellor for Research at Guilan University of Medical Sciences, Rasht, Iran, for approving and funding this research. The authors also thank their colleagues at the Babol Comprehensive Health Centers for their invaluable support, as well as all participants who generously volunteered their time and effort during this study.
References
- Neamati Vonashi R, Saliminia AR. [Comparison of dimensions of perfectionism and the source of health control in patients with obsessive-compulsive disorder (OCD) and depressed patients (Persian)]. Q Appl Psychol. 2019; 12(4):513-29. [Link]
- Metrics I. Evaluation, Global Health Data Exchange (GHDx). Institute of Health Metrics and Evaluation Seattla. 2021. [Link]
- World Health Organization (WHO). World mental health report: Transforming mental health for all [Internet]. 2022 [Updated 2022 June 16]. Available from: [Link]
- World Health Organization (WHO). Mental health and COVID-19: Early evidence of the pandemic’s impact. Geneva: World Health Organization; 2022. [Link]
- Santo L, Kang K. National ambulatory medical care survey: 2019 national summary tables. Hyattsville: National Center For Health Statistics; 2019. [DOI:10.15620/cdc:123251]
- World Health Organization (WHO). Mental health atlas Geneva: World Health Organization; 2020. [Link]
- Moitra M, Santomauro D, Collins PY, Vos T, Whiteford H, Saxena S, et al. The global gap in treatment coverage for major depressive disorder in 84 countries from 2000-2019: A systematic review and Bayesian meta-regression analysis. PLoS Med. 2022; 19(2):e1003901. [DOI:10.1371/journal.pmed.1003901] [PMID]
- Ghorbani V, Jandaghiyan M, Jokar S, Zanjani Z. [The prediction of depression, anxiety, and stress during the COVID-19 outbreak based on personality traits in the residents of Kashan City from March to April 2020: A descriptive study (Persian)]. J Rafsanjan Univ Med Sci. 2021; 20(5):503-18. [DOI:10.52547/jrums.20.5.503]
- Marijanović I, Pavleković G, Buhovac T, Martinac M. The relationship between health locus of control, depression, and sociodemographic factors and amount of time breast cancer patients wait before seeking diagnosis and treatment. Psychiatr Danub. 2017; 29(3):330-44. [DOI:10.24869/psyd.2017.330] [PMID]
- Trifiletti LB, Gielen AC, Sleet DA, Hopkins K. Behavioral and social sciences theories and models: Are they used in unintentional injury prevention research? Health Educ Res. 2005; 20(3):298-307. [DOI:10.1093/her/cyg126] [PMID]
- McAnena C, Craissati J, Southgate K. Exploring the role of locus of control in sex offender treatment. J Sex Aggress. 2016; 22(1):95-103. [DOI:10.1080/13552600.2015.1023374]
- Fallahzadeh H, Momayyezi M, Nikokaran J. [Prevalence of depression, anxiety and stress in Yazd (2013) (Persian)]. Tolooebehdasht. 2016; 15(3):155-64. [Link]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995; 33(3):335-43. [DOI:10.1016/0005-7967(94)00075-U] [PMID]
- Ali AM, Green J. Factor structure of the depression anxiety stress Scale-21 (DASS-21): Unidimensionality of the Arabic version among Egyptian drug users. Subst Abuse Treat Prev Policy. 2019; 14(1):40. [DOI:10.1186/s13011-019-0226-1] [PMID]
- Wallston KA, Wallston BS, DeVellis R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Monogr. 1978; 6(2):160-70. [DOI:10.1177/109019817800600107] [PMID]
- Moshki M, Ghofranipour F, Hajizadeh E, Azadfallah P. Validity and reliability of the multidimensional health locus of control scale for college students. BMC Public Health. 2007; 7:295. [DOI:10.1186/1471-2458-7-295] [PMID]
- Coker AO, Coker OO, Sanni D. Psychometric properties of the 21-item depression anxiety stress scale (DASS-21). African Research Review. 2018; 12(2):135-42. [DOI:10.4314/afrrev.v12i2.13]
- Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog Neuro Psychopharm Biol Psychiatry. 2021; 109:110236. [DOI:10.1016/j.pnpbp.2020.110236]
- Kavvadas D, Kavvada A, Karachrysafi S, Papaliagkas V, Cheristanidis S, Chatzidimitriou M, et al. Stress, anxiety and depression prevalence among Greek University students during COVID-19 pandemic: A two-year survey. J Clin Med. 2022; 11(15):4263. [DOI:10.3390/jcm11154263] [PMID]
- Nasirzadeh M, Akhondi M, Khorramnia S. [A survey on stress, anxiety, depression and resilience due to the prevalence of COVID-19 among Anar City Households in 2020: A short report (Persian)]. J Rafsanjan Univ Med Sci. 2020; 19(8):889-98. [DOI:10.29252/jrums.19.8.889]
- Nahidi M, Mirza HM, Tabesh H. [Prevalence of anxiety, depression, and stress, as well as their psychosocial correlates, among medical students during the COVID-19 pandemic (Persian)]. Med J Mashhad Univ Med Sci. 2023; 65(6):2293-309. [DOI:10.22038/mjms.2023.68881.4091]
- Barzideh M, Choobineh A, Tabatabaei H. [Job stress dimensions and their relationship to musculoskeletal disorders in nurses (Persian)]. Health Syst Res. 2012; 8(7): 1365-75. [Link]
- Molaeipour L, Hajebi A, Janani L, Salehi M, Taghdisi MH, Nazari-Kangavari H, et al. Monitoring the COVID-19 vaccine acceptance trend and its determinants among Iranian Adults. Arch Iran Med. 2023; 26(8):427-33. [DOI:10.34172/aim.2023.65] [PMID]
- Ganjoo M, Farhadi A, Baghbani R, Daneshi S, Nemati R. Association between health locus of control and perceived stress in college student during the COVID-19 outbreak: A cross-sectional study in Iran. BMC Psychiatry. 2021; 21(1):529. [DOI:10.1186/s12888-021-03543-1] [PMID]
- Alat P, Das SS, Arora A, Jha AK. Mental health during COVID-19 lockdown in India: Role of psychological capital and internal locus of control. Curr Psychol. 2023; 42(3):1923-35. [DOI:10.1007/s12144-021-01516-x] [PMID]
- Holden SL, Forester BE, Williford HN, Reilly E. Sport locus of control and perceived stress among college student-athletes. Int J Environ Res Public Health. 2019; 16(16):2823. [DOI:10.3390/ijerph16162823] [PMID]
- Khumalo T, Plattner IE. The relationship between locus of control and depression: A cross-sectional survey with university students in Botswana. S Afr J Psychiatr. 2019; 25:1221. [DOI:10.4102/sajpsychiatry.v25i0.1221] [PMID]
- Ghanbari-afra L, Ghanbari-afra M. [Occupational Stress of Nurses and its Related Factors During the COVID-19 Pandemic: A systematic review (Persian)]. Qom Univ Med Sci J. 2023; 16(10):774-785. [DOI:10.32598/qums.16.10.949.9]
- Shah SMA, Mohammad D, Qureshi MFH, Abbas MZ, Aleem S. Prevalence, psychological responses and associated correlates of depression, anxiety and stress in a global population, during the coronavirus disease (COVID-19) Pandemic. Community Ment Health J. 2021; 57(1):101-10. [DOI:10.1007/s10597-020-00728-y] [PMID]
- Zare M, Soleimani Ahmadi M, Eshaghi Sani H, Khademian M, Zare MR, Zomordi SH, et al. [Health Anxiety and Factors Affecting it in Housewives During the Covid-19 Pandemic (Persian)]. J Prev Med. 2022; 9(1):18-27. [Link]
- Gambin M, Sękowski M, Woźniak-Prus M, Wnuk A, Oleksy T, Cudo A, et al. Generalized anxiety and depressive symptoms in various age groups during the COVID-19 lockdown in Poland. Specific predictors and differences in symptoms severity. Compr Psychiatry. 2021; 105:152222. [DOI:10.1016/j.comppsych.2020.152222] [PMID]
- Lee H, Choi D, Lee JJ. Depression, anxiety, and stress in Korean general population during the COVID-19 pandemic. Epidemiol Health. 2022; 44:e2022018. [DOI:10.4178/epih.e2022018] [PMID]
- Karimi S, Andayeshgar B, Khatony A. Prevalence of anxiety, depression, and stress in patients with multiple sclerosis in Kermanshah-Iran: A cross-sectional study. BMC Psychiatry. 2020; 20(1):166. [DOI:10.1186/s12888-020-02579-z] [PMID]
- Zilver SJM, Broekman BFP, Hendrix YMGA, de Leeuw RA, Mentzel SV, van Pampus MG, et al. Stress, anxiety and depression in 1466 pregnant women during and before the COVID-19 pandemic: A Dutch cohort study. J Psychosom Obstet Gynaecol. 2021; 42(2):108-14. [DOI:10.1080/0167482X.2021.1907338] [PMID]
- Chen Y, Huang X, Zhang C, An Y, Liang Y, Yang Y, et al. Prevalence and predictors of posttraumatic stress disorder, depression and anxiety among hospitalized patients with coronavirus disease 2019 in China. BMC Psychiatry. 2021; 21(1):80. [DOI:10.1186/s12888-021-03076-7] [PMID]
- Nie XD, Wang Q, Wang MN, Zhao S, Liu L, Zhu YL, et al. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int J Psychiatry Clin Pract. 2021; 25(2):109-14. [DOI:10.1080/13651501.2020.1791345] [PMID]
- Pahlevan Sharif S, Ahadzadeh AS, Ong FS, Naghavi N. Fear of negative appearance evaluation and attitude towards mammography: Moderating role of internal health locus of control,cancer worry and age. Health Promot Perspect. 2020; 10(3):220-9. [DOI:10.34172/hpp.2020.35] [PMID]
- Miličić D, Brajković L, Ljubas Maček J, Andrić A, Ardalić Z, Buratović T, et al. Type a personality, stress, anxiety and health locus of control in patients with acute myocardial infarction. Psychiatr Danubina. 2016; 28(4):409-14. [Link]
- de Dios-Duarte MJ, Arias A, Durantez-Fernández C, Niño Martín V, Olea E, Barba-Pérez MÁ, et al. Flare-ups in crohn's disease: Influence of stress and the external locus of control. Int J Environ Res Public Health. 2022; 19(20):13131. [DOI:10.3390/ijerph192013131] [PMID]
- Cheng C, Cheung MW, Lo BC. Relationship of health locus of control with specific health behaviours and global health appraisal: A meta-analysis and effects of moderators. Health Psychol Rev. 2016; 10(4):460-77. [DOI:10.1080/17437199.2016.1219672] [PMID]
- Origlio J, Odar Stough C. Locus of control and pre-pandemic depressive symptoms relate to psychological adjustment of college students to the COVID-19 pandemic. J Am Coll Health. 2024; 72(2):522-29. [DOI:10.1080/07448481.2022.2047699] [PMID]
Article Type: Original Contributions |
Subject:
Health Education and Promotion
Received: 2024/12/19 | Accepted: 2025/02/11 | Published: 2025/04/21
Received: 2024/12/19 | Accepted: 2025/02/11 | Published: 2025/04/21
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |